Basics

What is Medicaid Managed Care?
Health Care
Published on September 10, 2019
Overview
Medicaid provides quality healthcare to over 75 million people in the United States, covering one in five low-income Americans. While the federal government requires states to cover certain populations and services, states have flexibility in deciding how to provide their benefits and how many people are eligible. States have traditionally utilized a fee-for-service (FFS) payment system to cover enrollees, but the share of Medicaid enrollees covered by the managed care model has increased dramatically since the 1990s.
In this basic, we break down what managed care means, its key components, as well as its enrollees, structure, and financing.
What is managed care?
Under Medicaid’s managed care model, enrollees receive most of their healthcare through an organization under contract with the state. Until the 1990s, states typically used a fee-for-service delivery model, or one where healthcare providers are paid by the state for each service provided to a patient.
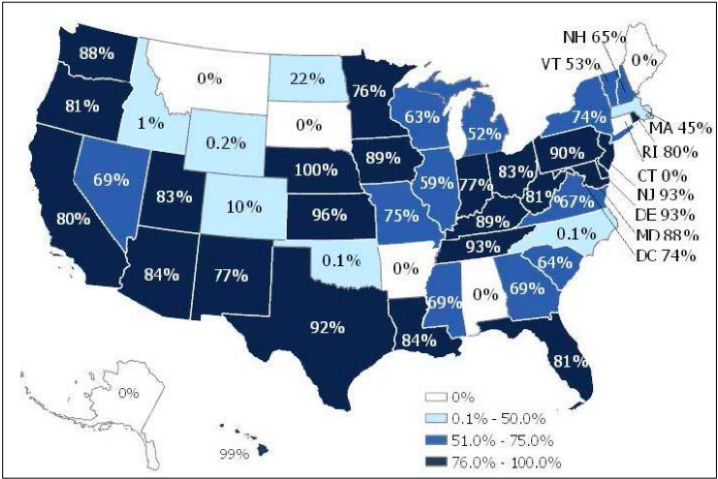
As of July 2017, about 82 percent of Medicaid enrollees were covered by some form of managed care. Since states have the ability to decide how best to provide coverage for their Medicaid populations, there is wide variation across the country in how services are delivered. The map below outlines the percentage of each state’s Medicaid population enrolled in a managed care plan in 2017.
Types of Managed Care
Comprehensive risk-based managed care
Of the three main types of Medicaid managed care, the most common is the comprehensive risk-based managed care provided through managed care organizations (MCOs). In 2017, 69 percent of Medicaid enrollees had this type of plan. In this model, states contract with MCOs to provide a full package of benefits to Medicaid enrollees. In turn, states typically pay the MCOs using a capitated payment system, or one where the MCO is paid a fixed monthly rate per enrollee to provide their healthcare services.
Primary care case management (PCCM)
In a PCCM model, states contract directly with primary care providers to provide case management services to Medicaid enrollees. The primary care provider usually receives a monthly case management fee per enrollee for coordinating care in addition to a fee-for-service payment for the medical services provided.
Limited benefit plans
Limited benefit plans are similar to MCOs in structure in that states typically contract with a plan and pay based on a capitated payment system. However, limited benefit plans only provide certain Medicaid services such as dental or behavioral health services instead of providing a full range of health services.
Why is managed care growing?
Comprehensive care
More and more states are adopting Medicaid managed care, particularly the use of MCOs. Of the 38 states employing managed care, 17 had at least 90 percent of their Medicaid population in MCOs. Managed care organizations are risk-based, meaning they are under contract with states to pay for enrollees’ care even if the costs exceed the capitated rates at which they are reimbursed. This arrangement encourages MCOs to invest in enrollees’ overall healthcare to avoid paying for more serious, costly treatments down the road.
In order to keep costs down, MCOs focus on the quality of care enrollees receive instead of the quantity of services, which is known as a value-based payment model. Achieving “value” can happen in a number of ways, such as tying provider payments to patient outcomes, implementing programs to address social determinants of health such as housing and food insecurity, and integrating physical and behavioral healthcare.
Expanding Medicaid population
In the past, states limited managed care arrangements to certain groups like children and pregnant women but they have increasingly expanded this approach to more enrollees, including those with complex medical needs. For instance, Medicaid is the primary payer for institutional and community-based long-term services and supports since there is limited coverage in Medicare. Seniors and people with disabilities make up 25 percent of Medicaid enrollees, yet account for almost two-thirds of program spending. States have increasingly shifted more enrollees onto managed care arrangements to control these costs.
Budgetary savings
States have also come to rely on managed care arrangements to provide state budget predictability. The price of care under a fee-for-service arrangement can be more volatile since the model incentivizes quantity over quality. Services may be uncoordinated or unnecessary, leading to needless costs incurred for Medicaid to reimburse.
How is it paid for?
Medicaid is structured as a partnership between the federal government and individual states and is therefore financed jointly by the two. The federal government reimburses states for the federal share of each state’s program costs and there is no cap or limit on the amount of federal funds a state can receive. The federal share of the bill is generally determined annually and varies by state according to each state’s per capita income relative to the U.S. per capita income; however, the federal reimbursement rate is at least 50 percent. In FY2018, Medicaid spent $616 billion, $386 billion of which was covered by the federal government and $230 billion of which was covered by states.
Looking Ahead
Medicaid enrollees consistently outperform the uninsured in access to care and rates of satisfaction among this group are comparable to those of Americans with private insurance. Research suggests that Medicaid eligibility during childhood is associated with improved long-run educational attainment and reduced disability. The Affordable Care Act allows for states to expand Medicaid to more low-income adults, which research shows has increased access to care and reduced mortality among this group. Additionally, states rely on Medicaid to cover treatment in disease outbreaks and crises, such as the Zika virus and the opioid epidemic.
Medicaid’s benefits are clear; however, it is still one of the most expensive line items in the federal budget. Medicaid accounted for 9.5 percent of federal spending in FY2017 and is the third-largest domestic program in the budget, after Social Security and Medicare. It was also the second-largest item in state budgets in 2017. Recognizing the importance of the program, policymakers are focused on containing costs and states have increasingly turned to managed care to do so. As policymakers debate reforms to Medicaid, expect to see states move more of their enrollees onto managed care arrangements.
Key Definitions
- Capitated payment model: Under this model, CMS, a state, and a health plan enter into a three-way contract to provide comprehensive, coordinated care.
- Centers for Medicare and Medicaid Services (CMS): Federal agency, in partnership with states, that covers over 100 million people through Medicare, Medicaid, Children’s Health Insurance Program (CHIP) and the Health Insurance Marketplace.
- Fee-for-service: Method of payment for medical services where the provider is paid for each service performed, i.e. office visit, blood work taken, tests administered, etc.
- Managed care organization (MCO): Health plan contracted with a state to provide health and additional services to beneficiaries on a predetermined per person, per month payment.
- Medicaid: Federal and state health coverage program that covers low-income families, qualified pregnant women and children and the elderly, as well as people with disabilities. In FY2016, 76 million Americans received health care coverage through Medicaid.
- Value-based arrangement: Payment mechanism whereby providers get paid or incentivized not necessarily by each individual service they provide (see fee for service) but rather for a broader treatment plan. This is a key part of the ACA and mechanisms like bundled payments and increased care coordination are examples of value-based arrangements.
A full glossary of common health care terms can be found HERE.